Washington, DC—In testimony today before the House Energy and Commerce Committee’s Subcommittee on Health, Raynard Washington, PhD, MPH, Health Director for Mecklenburg County (serving Charlotte, NC, and surrounding communities) and Vice Chair of the Big Cities Health Coalition, will provide a frontline, local governmental public health perspective on the critical importance of reauthorizing the Pandemic and All-hazards Preparedness Act (PAHPA).
The hearing, “Legislative Solutions to Bolster Preparedness and Response for All Hazards and Public Health Security Threats,” will examine “solutions for preparedness and response to public health security threats and hazards.”
“Reauthorization of PAHPA is key to ensuring that the infrastructure necessary to prepare and respond to the ever-evolving health threats we encounter at the local level,” Dr. Washington shares in his testimony today.
Watch clips from Dr. Washington’s testimony
Key points include:
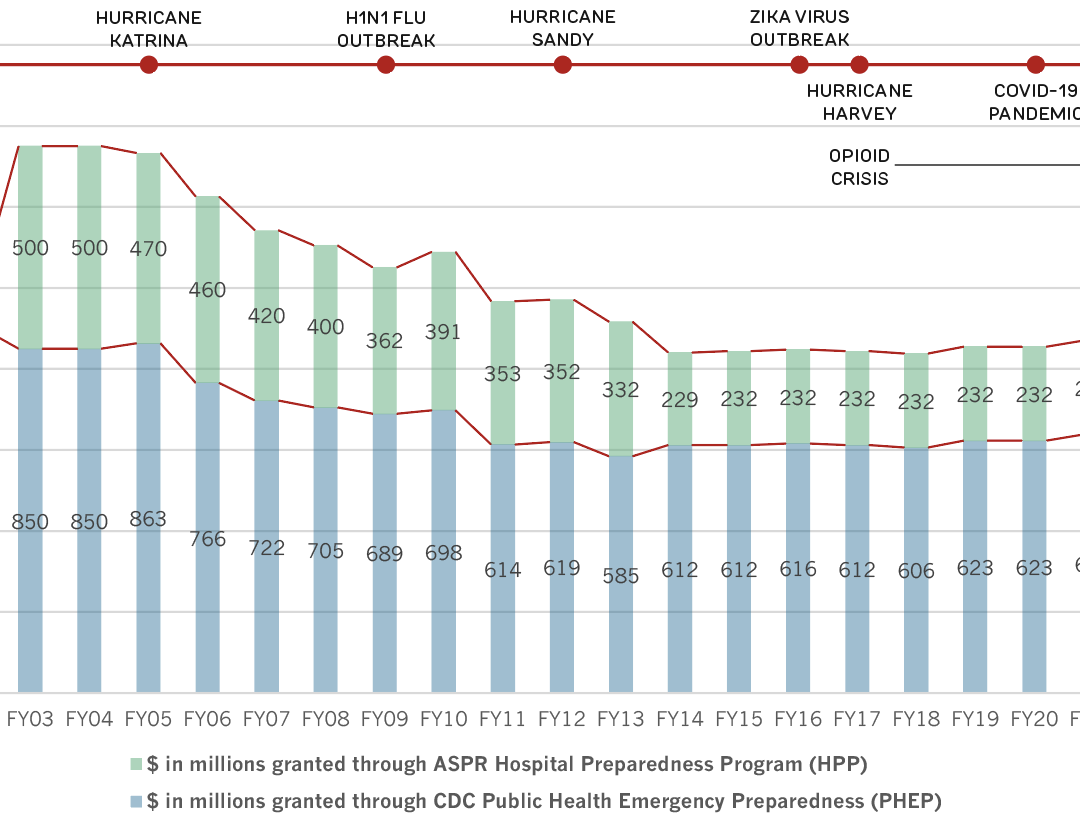
- Public Health Emergency Preparedness Program (PHEP): “PHEP is critical to having a response-ready workforce at the local level. In Mecklenburg County, our health department preparedness staff has grown from 1 FTE to 3 since the start of COVID-19 due to federal investments…. These funds allow us to train staff and maintain and implement local response plans for every type of hazard…. Unfortunately, PHEP funding to grantees has been cut by nearly 30 percent over the last two decades, despite the increase in emerging and re-emerging infectious diseases, and weather-related, environmental, and other emergencies and disasters.”
- Hospital Preparedness Program (HPP): “HPP supports regional health care coalitions, like the Metrolina Healthcare Preparedness Coalition in our region [Mecklenburg County], to incentivize health care readiness, assess risks and needs, train the workforce, and maintain preparedness among organizations that might otherwise see each other as competitors. As such, HPP is a vital support – but it has been cut by more than 50 percent over the last 20 years and remains stretched due to prolonged emergency responses, increased preparedness and response requirements, and annual discretionary funding not keeping pace with inflation.”
- Epidemiology and Laboratory Capacity (ELC): “Our department, like many across the country, relied heavily on ELC funding we received through [funding to the state of] North Carolina, to support our daily COVID-19 response activities, including additional staff capacity to support epidemiology, data reporting, case investigation, contact tracing and testing. Despite ELC’s vital role in responding to the pandemic, annual funding levels are not adequate to maintain public health preparedness or address routine challenges.”
- Adult Vaccine Program: “While the existing National Vaccine Program, or 317, is a critical support mechanism, it is not sufficiently funded to support vaccination for all uninsured and underinsured adults. [A new adult vaccine] program is essential for enhancing and maintaining the infrastructure needed for future pandemic response, while also ensuring access to routine vaccines in non-emergencies.”
- CDC Data Authority: “CDC should be given the authority to effectively collect and coordinate public health data necessary to serve its mission. The current framework for collecting and sharing public health data has resulted in fragmented and inconsistent reporting to CDC, and to state and local public health partners. Expanded data authority for CDC will allow for more complete and timely data sharing to support decisions at the federal, state, and local levels, while reducing burden on providers.”
- Federal Funding: “Effective public health response depends on action at the federal, state, tribal, local, and territorial levels of government – and each level of government needs to be appropriately resourced in as direct and timely a manner as possible. CDC should continue – and should be encouraged by Congress – to broaden its direct grantmaking pool to include, at a minimum, the 107 jurisdictions funded under the Public Health Infrastructure and Workforce Development Grant Program. It is essential that funding for emergency preparedness and response, disease detection, and surveillance reaches those on the ground that are the first to identify and respond to health security threats.”
Dr. Washington brings to the hearing more than 15 years in governmental public health. Before becoming Health Director, he was the Deputy Director in Mecklenburg County, and before that was Chief Epidemiologist and Deputy Health Commissioner at Philadelphia’s Department of Public Health. He holds a doctorate in epidemiology, a field that focuses on the incidence, distribution, and control of diseases and other health factors.
About the Big Cities Health Coalition
The Big Cities Health Coalition (BCHC) is a forum for the leaders of America’s largest metropolitan health departments to exchange strategies and jointly address issues to promote and protect the health and safety of their residents. Collectively, BCHC member jurisdictions directly impact more than 61 million people, or one in five Americans. For more information, visit bigcitieshealth.org.