Frontline Blog
Now is the Time to Tell Policymakers that Trauma Matters to Our Health
January 2019
By Kelly Colopy, MPP, BCHC Chair and Director, Long Beach Health Department Director
and Amanda Merck, MPH, Senior Research Area Specialist, Salud America!, UT Health San Antonio
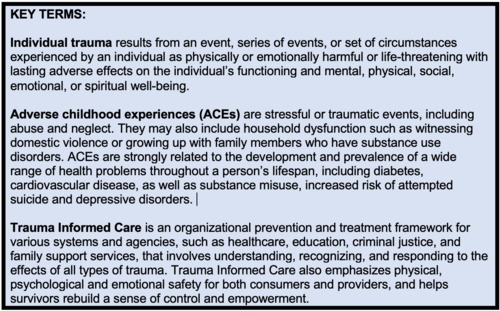
Public health professionals all over the country are leveraging practice and policy strategies to address the issue of trauma, including incorporating a “trauma-informed” point of view into the way they conduct business. In recent years, public health science and practice has become more cognizant of the evidence of, and action needed, to support those who suffer from trauma. This awareness and response is starting to transform the field.
Today, we are calling on our dedicated public health colleagues to leverage your knowledge and urge federal lawmakers to acknowledge and incorporate trauma into the way they do business.
Now through next Thursday, January 17th, the U.S. Department of Health and Human Services (HHS) is soliciting written comments regarding the Healthy People 2030 objectives. Every decade, the Healthy People initiative develops a new set of evidence-based, 10-year national objectives with the goal of improving the health of all Americans. This year, HHS sought to streamline the objectives. Unfortunately, a specific type of trauma called Adverse Childhood Experiences (ACEs) are not currently included in the newly proposed objectives.
Taking Action
We need public health leaders to elevate ACEs on the national public health agenda by urging HHS to address childhood trauma in the Healthy People 2030 proposed objectives. Salud America! crafted three quick-and-easy opportunities to provide written comments.
It’s been 20 years since the original ACEs Study, done by Kaiser Permanente. We can’t wait another 10. If a person has six or more ACEs, that person is more likely to die 20 years earlier than someone with no ACEs.
Why? Chronically high levels of cortisol and adrenaline during childhood affect the brain and are associated with reduced neural connections in the area of the brain dedicated to learning and reasoning; decreased ability to interpret social cues and language; and decreased ability to sleep, breathe, relax, and cope with future adversity. ACEs, stressors, as well as risky coping behaviors, and physical ailments are associated with increasing these hormones. High levels of stress hormones during childhood also affect the body and are associated with increased blood sugar, blood pressure, inflammation, and decreased immunity.
Children who experience chronic or severe trauma are at an increased risk for diabetes, heart disease, autoimmune disease, asthma, cancer, anxiety, depression, substance abuse, homelessness, dropping out of high school, and involvement in the criminal justice system.
Preventing ACEs and helping children cope with adversity can improve health and well-being over their lifespan, reduce premature death, and reduce healthcare costs in our cities. According to a 2012 study, lifetime costs due to child maltreatment in the United States was approximately $124 billion each year in child and adult medical costs, productivity losses, child welfare, criminal justice and special education costs. Additional ACEs only increase these costs.
This is why cities across the country are working to combat ACEs, below you’ll learn more about what Long Beach, CA is doing.
How One Health Department is Leading
At the Long Beach Department of Health and Human Services, we have seen, first hand, the impact on health and well-being of not only ACEs, but also trauma after childhood. We began implementing trauma informed efforts in 2015, with an understanding that many of the people living in our communities have experienced personal and community-level trauma either in childhood or throughout their lives. This impacts their ability to learn, grow, react in situations as well as their overall health and well-being. As a department, we understand that almost all of those who walk in our door have experienced trauma. It is essential that we recognize this and operate from a trauma informed approach which starts with a simple reframing of a question. We train people to no longer ask “What’s wrong with you?” Instead, we now ask, “What happened to you?” This begins an important conversation and better understanding for next steps.
We also understand that across our city, many departments and systems such as the schools, parks and recreation, and emergency services have daily interactions with people who have or are experiencing trauma, and we have the potential to re-traumatize them without fully understanding the impact. We are acting to change this:
- In 2015 and 2016, the City trained over 1,300 City and community partners and implemented a Trauma Informed Awareness Campaign. This initiative included trainings for our staff that delivered a greater understanding of the physical, emotional and behavioral symptoms associated with trauma exposure, and how to leverage a trauma-informed approach in our day-to-day work.
- Simultaneously, in 2015, the City launched The Long Beach Trauma and Resiliency Informed Taskforce, which spent 15 months planning and developing an action plan for a Trauma Informed Long Beach. This work includes piloting trauma and resiliency strategies within and across our systems, and convening key champions to design and implement strategies to boost resiliency.
- And, for the next two years we’ll continue the work of developing and strengthening a cross-systems and citywide trauma and resiliency informed approach to address the concerns in communities with high rates of trauma.
Many traumas can be identified early using systematic surveillance and screening, which can inform necessary care and services. However, many state and local health departments lack such systems. Between 2011 and 2014, only 23 states included ACEs items in the Behavioral Risk Factor Surveillance System (BRFSS). Researchers analyzed data from these 23 states and found that the variation of ACEs across demographic groups supports literature showing that social and structural conditions contribute to the risk of exposure to childhood adversity and that exposure to ACEs may exacerbate inequities in health, social, and economic outcomes across generations.
In school, for example, if subjected to chronic, severe, unpredictable stress, a child may experience either hyperarousal or hypoarousal and in a state of fight, flight, or freeze, which compromises their cognitive and socioemotional development and thus their ability to learn. Children in these states often disrupt the learning of others and face disciplinary action.
It starts young. Preschoolers are facing in-school and out-of-school suspension, which denies them valuable learning time and does nothing to build resilience. Suspended students are more likely to have poor grades, continue misbehaving, and drop out of school, which worsens health inequities for these kids who are already at risk due to the initial traumatic experiences.
As trauma expert Dr. Joe Hendershott says, these kids are beyond “at-risk.” They are wounded. Hendershot has inspired educators across the country to learn a new way, a trauma-informed way, to understand and connect with these students.
Using What We Know Works and Taking Action
It is important that all our cities be equipped like Long Beach to talk about life-altering wounds and provide trauma-informed care, that pediatricians are equipped to advise foster parents to consider past abuse in understanding how foster children may respond to different disciplinary strategies; that school counselors are equipped to work more closely with teachers and assistant principals to handle misbehavior and absenteeism and help build student’s resilience; and that Public health departments are equipped to work across health care systems, family support services, and schools to coordinate trauma-informed care.
This is why it’s such a problem that the proposed objectives for Healthy People 2030 do not address “adverse childhood experiences.” The term “childhood trauma” is found zero times in 63 pages. Including objectives that address childhood trauma in Healthy People 2030 would be a critical step to elevate ACEs on the national health agenda.
You have until Jan. 17 to speak up to make ACEs and childhood trauma a priority for Healthy People 2030. Act now!